Shockwave therapy has become an increasingly popular treatment option for a variety of medical conditions, ranging from musculoskeletal problems like tendonitis and plantar fasciitis to more complex issues such as Peyronie's disease. One of the most common questions patients have when considering this treatment is whether their insurance will cover the cost. In this blog post, we'll explore the ins and outs of insurance coverage for shockwave therapy, with a particular focus on the use of low intensity shockwave therapy machine.

Understanding Shockwave Therapy and Low Intensity Shockwave Therapy Machines
Shockwave therapy involves the use of high - energy sound waves to stimulate the body's natural healing processes. These shockwaves can be delivered at different intensities, and a low intensity shockwave therapy machine is designed to provide a more gentle form of treatment. The low intensity shockwaves are still effective in promoting tissue repair, reducing inflammation, and breaking down scar tissue, but they are often considered a more conservative approach.
For example, in the treatment of chronic tendon injuries, a low intensity shockwave therapy machine can be used to target the damaged tendon area. The shockwaves penetrate the tissue, causing a series of physiological responses. They stimulate the production of new blood vessels, which improves blood flow to the area, and also encourage the regeneration of cells. This helps the tendon to heal more effectively.
Insurance Coverage Basics
Insurance coverage for medical treatments, including shockwave therapy, depends on several factors. Insurance providers typically base their decisions on whether a treatment is considered "medically necessary." Medical necessity is determined by whether the treatment is appropriate, reasonable, and required for the diagnosis or treatment of an illness or injury.
For shockwave therapy to be covered by insurance, it often needs to be prescribed by a licensed healthcare provider for a condition that is recognized by the insurance company as treatable with this method. However, different insurance plans, whether they are private health insurance, Medicare, or Medicaid, have their own specific guidelines and policies regarding shockwave therapy coverage.
Private Health Insurance and Low Intensity Shockwave Therapy Machines
Private health insurance companies vary widely in their coverage of shockwave therapy. Some may cover the cost of treatments using a low intensity shockwave therapy machine if the treatment is for a condition such as a severe tendonitis that has not responded to other conservative treatments like physical therapy and medication.
For instance, if a patient has been suffering from tennis elbow for months and has tried rest, anti - inflammatory drugs, and physical therapy without significant improvement, their doctor may recommend shockwave therapy using a low intensity shockwave therapy machine. In such a case, the insurance company may consider covering the treatment as it is seen as a necessary step in the patient's treatment plan.
However, other private insurers may be more restrictive. They may require prior authorization before covering the treatment. This means that the doctor must submit a detailed treatment plan to the insurance company, explaining why shockwave therapy with a low intensity shockwave therapy machine is the best option for the patient. The insurance company will then review the request and decide whether to approve the coverage.
Medicare and Medicaid Coverage
Medicare, which provides health insurance for people aged 65 and older, as well as some younger people with disabilities, has specific rules regarding shockwave therapy. In general, Medicare may cover shockwave therapy for certain conditions, but again, it must meet the criteria of medical necessity.
For example, for patients with plantar fasciitis who have not responded to at least six months of conservative treatment, Medicare may cover shockwave therapy using a low intensity shockwave therapy machine. However, the treatment must be provided in a Medicare - approved facility, and the healthcare provider must follow all Medicare regulations.
Medicaid, which provides health coverage for low - income individuals and families, also has its own set of rules. Medicaid programs vary from state to state, so the coverage of shockwave therapy using a low intensity shockwave therapy machine can differ significantly depending on where the patient lives. Some states may cover shockwave therapy for a limited number of conditions, while others may not cover it at all.
Factors Affecting Insurance Coverage
Several factors can influence whether insurance will pay for shockwave therapy using a low intensity shockwave therapy machine. The first is the diagnosis. As mentioned earlier, the condition being treated must be recognized by the insurance company as a valid indication for shockwave therapy. For example, if a patient has a rare condition that is not commonly treated with shockwave therapy, the insurance company may be less likely to cover the treatment.
The second factor is the location of the treatment. Insurance companies may only cover shockwave therapy if it is provided in an in - network facility. Using an out - of - network provider can result in higher costs for the patient, as the insurance company may not cover the full amount or may not cover it at all.
The frequency and duration of the treatment also matter. Insurance companies may limit the number of shockwave therapy sessions they will cover. For example, they may only pay for a maximum of six sessions using a low intensity shockwave therapy machine for a particular condition. If the patient requires more sessions, they may have to pay out - of - pocket for the additional treatments.
Documentation and Pre - Authorization
To increase the likelihood of insurance coverage for shockwave therapy with a low intensity shockwave therapy machine, proper documentation is crucial. The healthcare provider must document the patient's medical history, the diagnosis, the reasons why shockwave therapy is being recommended, and the expected outcomes of the treatment.
In addition, as mentioned earlier, many insurance companies require pre - authorization. This involves submitting a detailed treatment plan to the insurance company before the treatment begins. The treatment plan should include information about the type of low intensity shockwave therapy machine that will be used, the number of sessions, and the expected cost. The insurance company will review this information and determine whether to approve the coverage.
Case Studies of Insurance Coverage
Let's look at some case studies to better understand how insurance coverage for shockwave therapy with a low intensity shockwave therapy machine works. Case 1: A 55 - year - old patient with chronic shoulder tendonitis had tried various treatments including physical therapy and corticosteroid injections without success. Their doctor recommended shockwave therapy using a low intensity shockwave therapy machine. The doctor submitted a detailed treatment plan to the patient's private insurance company, explaining the medical necessity of the treatment. The insurance company approved the coverage, and the patient was able to receive the recommended number of shockwave therapy sessions.
Case 2: A 70 - year - old Medicare patient with severe plantar fasciitis had been suffering for over a year. After six months of conservative treatment, their doctor prescribed shockwave therapy using a low intensity shockwave therapy machine.
The treatment was provided in a Medicare - approved facility, and all the necessary documentation was submitted. Medicare covered the cost of the treatment, allowing the patient to start on the path to recovery.
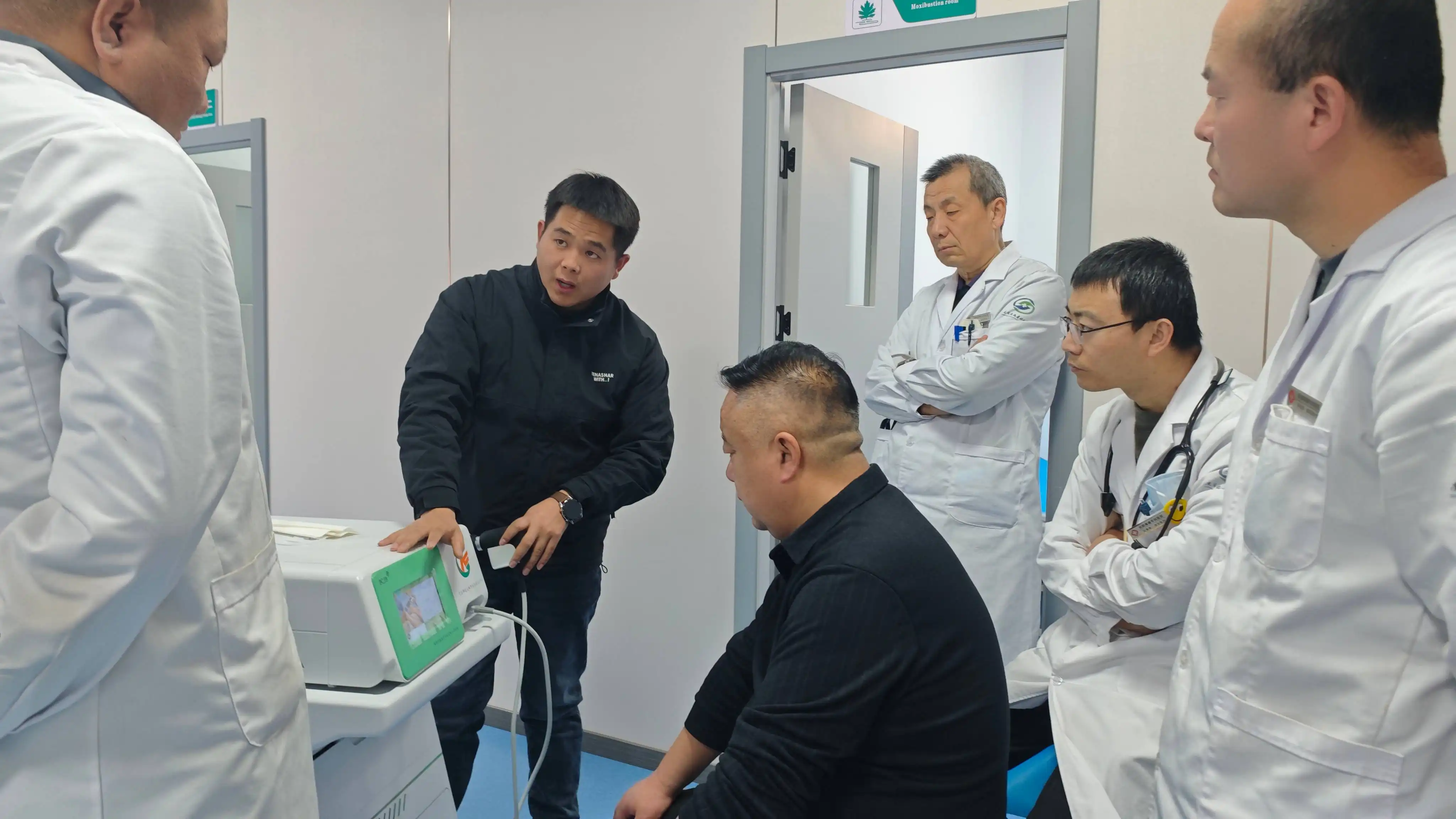
Shaanxi Miaokang Medical Technology Co., Ltd had R&d and produce low intensity shockwave therapy machine
is a comprehensive integrator engaged in medical instrument research and development, sales, medical technology research and promotion, and investment in medical institutions. The main research and development of medical ozone therapy equipment, extracorporeal shock wave therapy equipment and other products.
If you had any questions,feel free to contact us:Cathy@miaokang.ltd
In conclusion, whether insurance pays for shockwave therapy using a low intensity shockwave therapy machine depends on a variety of factors, including the type of insurance, the diagnosis, the location of the treatment, and proper documentation. It's important for patients to work closely with their healthcare providers and insurance companies to understand their coverage options and to ensure that they receive the best possible treatment for their condition.






