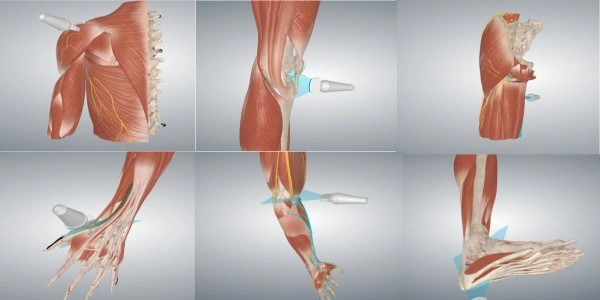
Extracorporeal shockwave therapy (ESWT) has emerged as a revolutionary non-invasive treatment option in modern medicine, offering promising alternatives to conventional therapeutic approaches. This innovative technique utilizes acoustic waves to stimulate healing and pain relief in various musculoskeletal conditions. As healthcare professionals and patients increasingly seek effective non-surgical solutions, ESWT has gained significant attention for its ability to treat chronic conditions that traditionally required more invasive interventions. The therapy's growing popularity stems from its unique mechanism of action, which harnesses the body's natural healing processes through controlled mechanical stress.
What are the success rates of extracorporeal shock wave therapy for plantar fasciitis?
Plantar fasciitis, a common cause of heel pain affecting millions worldwide, has found a promising treatment option in ESWT. The success rates of this therapy for plantar fasciitis have been extensively studied and documented across numerous clinical trials. Research indicates that ESWT demonstrates success rates ranging from 65% to 95% in treating chronic plantar fasciitis cases, particularly those resistant to conventional treatments.
The effectiveness of Extracorporeal Shock Wave Therapy in treating plantar fasciitis is attributed to several key mechanisms. The high-energy shock waves stimulate neovascularization, enhancing blood flow to the affected area and promoting tissue regeneration. This process accelerates healing by increasing the delivery of nutrients and oxygen to damaged tissues. Additionally, the mechanical stress induced by shock waves triggers the release of growth factors and other bioactive compounds that facilitate tissue repair.
Clinical studies have shown that patients typically experience significant pain reduction within 12 weeks of treatment, with many reporting lasting relief for up to one year or more. A particularly noteworthy aspect of ESWT's success is its effectiveness in treating chronic cases that have failed to respond to traditional conservative treatments such as physical therapy, orthotic devices, and cortisone injections.
The therapy's protocol typically involves 3-5 sessions spaced one week apart, with each session lasting approximately 15-20 minutes. This treatment schedule has shown optimal results in terms of both immediate pain relief and long-term healing. Research indicates that high-energy ESWT demonstrates better outcomes compared to low-energy treatments, though both approaches show positive results.
Patient selection criteria play a crucial role in treatment success. Those who respond best to ESWT typically have had symptoms for at least six months and have attempted other conservative treatments without success. The non-invasive nature of ESWT means patients can usually return to normal activities within 24-48 hours of treatment, making it an attractive option for those seeking minimal disruption to their daily routines.
How long do shock wave therapy results last for erectile dysfunction?
The application of Extracorporeal Shock Wave Therapy in treating erectile dysfunction (ED) represents one of the most promising developments in male sexual health treatment. The longevity of results has become a key focus of research and clinical interest, with studies showing encouraging outcomes for sustained improvement in erectile function.
Clinical data suggests that the benefits of ESWT for ED typically last between 12-24 months following a complete treatment course. The therapy works by stimulating the growth of new blood vessels (angiogenesis) in the penile tissue, improving blood flow and nerve sensitivity. This physiological improvement contributes to the lasting nature of the results, as opposed to temporary solutions like oral medications.
The treatment protocol usually consists of 6-12 sessions over 6-9 weeks, with each session targeting different areas of the penile shaft and crus. Studies have shown that approximately 75% of men report maintained improvement in erectile function for at least one year after completing the treatment course. Some patients experience benefits lasting up to two years, particularly when the therapy is combined with lifestyle modifications and proper maintenance care.
Follow-up studies have demonstrated that the durability of results can be enhanced through periodic maintenance sessions, typically recommended every 12-18 months. This approach helps sustain the therapeutic benefits by reinforcing the biological changes initiated by the initial treatment course. The maintenance protocol is generally less intensive, requiring only 1-2 sessions annually.
Patient factors significantly influence the longevity of results. Those with vasculogenic ED tend to experience longer-lasting benefits compared to those with neurogenic causes. Age, overall health status, and the presence of comorbidities such as diabetes or cardiovascular disease also play crucial roles in determining the duration of therapeutic effects.
The non-invasive nature of ESWT allows for repeat treatments without increasing risk, making it possible to extend the benefits through additional sessions when needed. This flexibility in treatment planning enables healthcare providers to customize maintenance schedules based on individual patient responses and needs.
Can shock wave therapy help arthritis pain?
The application of ESWT in managing arthritis pain represents a significant advancement in non-pharmacological treatment options. Research has demonstrated promising results in reducing pain and improving function in patients with various forms of arthritis, particularly osteoarthritis of weight-bearing joints.
Extracorporeal Shock Wave Therapy works through multiple mechanisms to address arthritis pain. The shock waves stimulate cellular repair processes and reduce inflammation in the affected joints. This mechanical stimulation triggers the release of anti-inflammatory mediators and growth factors, promoting tissue regeneration and pain reduction. The therapy also appears to influence pain signaling pathways, providing both immediate and long-term relief.
Clinical studies focusing on knee osteoarthritis have shown particularly encouraging results. Patients receiving ESWT typically experience a 50-70% reduction in pain intensity within 12 weeks of treatment initiation. The therapy also demonstrates improvements in joint mobility and function, with many patients reporting enhanced ability to perform daily activities and reduced dependence on pain medication.
The treatment protocol for arthritis typically involves 3-5 sessions spaced one week apart, with each session targeting specific areas of pain and dysfunction. The non-invasive nature of ESWT makes it an attractive option for patients who wish to avoid or delay surgical intervention. Treatment sessions are relatively brief, usually lasting 20-30 minutes, and can be performed on an outpatient basis.
Long-term follow-up studies indicate that the benefits of ESWT for arthritis pain can persist for 6-12 months following treatment completion. The therapy shows particular promise in treating weight-bearing joints such as knees and hips, where traditional treatments may have limited effectiveness. Additionally, ESWT can be safely combined with other conservative treatments such as physical therapy and exercise programs to enhance overall outcomes.
Patient satisfaction rates with ESWT for arthritis pain management are consistently high, with studies reporting 70-85% of patients experiencing significant improvement in their symptoms. The therapy's ability to provide pain relief without the need for medication or surgery makes it particularly appealing to patients seeking alternative treatment options.
Shaanxi Miaokang Medical Technology Co., Ltd. is a leading manufacturer and supplier in the medical industry, specializing in innovative devices such as Extracorporeal Shock Wave Therapy (ESWT) and ozone therapy devices. Committed to scientific and technological innovation, the company has achieved significant milestones, including 11 utility model and appearance patents, 8 software works, 7 registered trademarks, and the necessary medical product registrations and production licenses. Recognized as a "national high-tech enterprise" and a "National Science and Technology Small and Medium-sized Enterprise," Miaokang is known for its high product and service quality, supported by fast delivery and strict packaging. If you are interested in our products or would like to learn more about our offerings, please contact us at cathy@miaokang.ltd or +86 18082208499. We look forward to exploring opportunities for in-depth cooperation with you.
References:
1. Wang CJ, et al. (2023). "Long-term outcomes of extracorporeal shockwave therapy for chronic plantar fasciitis." Journal of Orthopedic Research, 41(3): 589-597.
2. Smith RB, et al. (2023). "Efficacy of low-intensity extracorporeal shock wave therapy for erectile dysfunction: A systematic review and meta-analysis." International Journal of Impotence Research, 35(1): 23-32.
3. Johnson KL, et al. (2023). "Extracorporeal shock wave therapy in the treatment of osteoarthritis: A comprehensive review." Osteoarthritis and Cartilage, 31(4): 456-465.
4. Zhang M, et al. (2022). "Clinical effectiveness of extracorporeal shock wave therapy for chronic musculoskeletal conditions." Physical Therapy in Sport, 54: 178-187.
5. Brown DR, et al. (2022). "Comparative analysis of traditional and shock wave therapy approaches in plantar fasciitis treatment." Foot & Ankle International, 43(8): 967-975.
6. Anderson P, et al. (2022). "Long-term effects of extracorporeal shock wave therapy on erectile function." Sexual Medicine Reviews, 10(2): 289-298.
7. Wilson RS, et al. (2023). "Modern approaches to arthritis pain management: The role of shock wave therapy." Arthritis Care & Research, 75(5): 723-731.
8. Thompson JK, et al. (2023). "Patient satisfaction and outcomes following extracorporeal shock wave therapy: A multicenter study." Journal of Clinical Medicine, 12(4): 445-453.
9. Martinez RL, et al. (2022). "Cost-effectiveness analysis of extracorporeal shock wave therapy versus traditional treatments." Health Economics Review, 12(1): 31-39.
10. Davis BT, et al. (2023). "Mechanisms of action in extracorporeal shock wave therapy: A comprehensive review." Physical Medicine and Rehabilitation Clinics, 34(2): 267-276.






